Psychedelics – The Panacea for the Ills of the Mind?
.jpeg)
By: Coco Bryant & Eriona Hysolli, PhD
ARTIS Fellows Class of 2021
It is estimated that the cost of mental health treatments in the U.S. alone is $200 billion, with just as much lost in earnings per year. Drugs, therapy, ECT, lifestyle changes, meditation, homeopathic solutions, social support groups, and self-help are all available for treatment with complete to zero recovery rates.
The mental health statistics speak for themselves, highlighting the urgency of this crisis and reflecting the deep-seated problems within this area of health, including low investment in preventative care and a lack of innovation in psychiatry. Nearly one in five adults in the United States lives with a mental illness, suicide is the tenth leading cause of death overall and the second leading cause of death for individuals between the ages of 10 and 34. Neuropsychiatric disorders are the leading cause of disability in the U.S. and ~30% of patients are resistant to currently available treatments. As it’s been widely reported, the COVID-19 pandemic further deepened the mental health crisis with the CDC reporting that between August 2020 and February 2021, the percentage of adults with recent symptoms of anxiety or depression increased from 36.4% to 41.5%, with the largest unmet mental health needs rising the most (7.2 percentage points) among adults ages 18 – 29 years.
With little hope for people struggling with treatment-resistant depression, post traumatic stress disorder, crippling anxiety and substance addiction, and no wonder-drugs available in the current standard of care, what are the medical alternatives? Psychedelic treatment has been growing in popularity and being increasingly discussed in the mainstream media - but what is the science and hype about?
Back to Basics
First let's get the basics down. Psychedelics are psychoactive substances that alter the mood, behavior and perception of reality during the “trip.” Visions, spiritual awakening, and overwhelming feelings of empathy and universal connectedness are commonly reported. The history of these compounds is long and dense with colorful stories and anecdotes. Psychedelic compounds have been extensively used by native tribes of Central and South America, and Africa in religious rituals and ceremonies. The natives used these compounds directly from their natural sources, more prominently psilocybin (derived from magic mushrooms), mescaline (peyote cactus), DMT and 5-MeO-DMT (ayahuasca brew and Sonoran desert toad) and ibogaine (Tabernanthe iboga shrub).
Psychedelics evolved and became more accessible after the discovery of chemical synthesis, which brought about not only the synthesized versions of the natural psychedelics, but also compounds like LSD, MDMA, ketamine and many others. LSD was first synthesized in 1938 by Swiss chemist Albert Hoffman to prevent blood loss in childbirth. It wasn’t until 1943 when Hofmann accidentally ingested a microscopic amount of lysergic acid through his skin that he became aware of its psychedelic properties as he rode his bike home (now known as the “Bicycle Day for the aficionados”).
During the 50s and 60s Richard Alpert and Timothy Leary characterized the hallucinogenic effects of psychedelics. Scientists published more than 1000 articles on using psychedelics as a psychiatric treatment of mood disorders and alcohol dependence, testing the compounds on ~40 000 people in total and showing initial therapeutic promise. However, when LSD became the symbol of the hippie counterculture in the 1960s, psychedelics soon became the target of the “War on Drugs” policies, and further psychedelic research was halted until the mid-1990s, but subsequently revived in academic labs and non-profit organizations like Johns Hopkins Center for Psychedelic and Consciousness Research, MAPS, Beckley Foundation/Imperial College London Psychedelic Research Program and Mount Sinai Center for Psychedelic Research. Psychedelics are still largely categorized as Schedule I controlled substances across America today.
Psychedelics for Mental Health
A landmark paper showing anti-depressant effects of ketamine in depressed patients published in 2000 was a game changer for psychedelic research. Today there are clinical trials on each of the psychedelic compounds for treatment of depression, PTSD, anxiety, and alcohol and opioid dependency disorders, consistently finding improvements compared to current standard of care. The tide is turning in the legalization battle as Oregon became the first state to legalize psilocybin-assisted therapy in 2020, with a few other states following as depicted in the map below.
.webp)
What makes psychedelics so effective for the treatment of mental health disorders? To start, we must first understand the physiological cause of the disorder. Let's take depression for example. We know that atrophy (death) of neurons in the prefrontal cortex (PFC) of the brain plays a key role. The stress that we all experience far too frequently in this modern world exacerbates the damage to these key neuronal pathways. Clinical data from studies show that multiple pathways responsible for the symptoms of depression arise from their neuroplasticity, in other words, how well neurons survive, adapt and grow.
Psychedelics are exceptionally good at promoting neuroplasticity in cortical neurons and the “rewiring” of the brain. The Default Mode Network (DMN) region of the brain is normally responsible for autobiographical, episodic and semantic memory, mind wandering, perspective-taking or future thinking. In depressed patients, the DMN is very active, which leads to classic symptoms like ruminations or loops of inward thinking. At the neurobiological level, psychedelics are able to normalize this activity, and increase connections to other areas of the brain that normally hit the brakes if the DMN is in overdrive.
Peer-reviewed research, blockbuster potential for treatment of mental disorders, and widespread coverage in popular culture have amplified the psychedelic message. A slew of recent psychedelic companies making successful IPO debuts is a clear indication that clinicians, public health experts, patients and investors are ready for radically good alternatives.
“Psychedelics for psychiatry and psychology [is] comparable to the value the microscope has for biology and the telescope has for astronomy”
(Stanislav Grof, 2015)
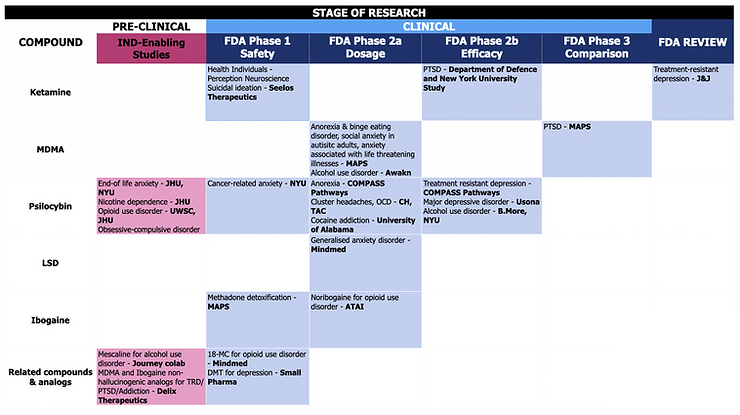
Mental health medications sales are estimated to be worth $100 billion, with FDA-approved psychedelic-assisted therapy for treatment-resistant depression alone carving out $10 billion. Psychedelic companies with the largest market caps include ATAI Life Sciences (market cap $2.4 billion), COMPASS ($1.4 billion), MindMed ($1 billion) and Field Trip Health ($300 million), with venture capital firms jumping at companies with patentable products and well-thought-out reimbursement strategies. A current tabulated summary of the clinical trials for various psychedelics conducted by select companies is shown below.
If you have perceptively asked about potential side effects, and the inevitable “trip” in order to achieve the therapeutic effect, you’ve hit on the main concerns for making psychedelic-assisted therapies scalable and accessible. The good news is that psychedelics are not a mystery to users and scientists, and overdosing and developing addiction is uncommon. Feelings of paranoia, and the triggering of manias in some bipolar patients are observed, though mostly because of the hallucinogenic activity. The more serious effect is cardiotoxicity. Most psychedelics use the 5-HT2A receptor for their neuropsychological effects, but cross-reaction with another receptor, 5-HT2B found in the heart, can lead to cardiac adverse effects. The other major challenge is providing these new therapies widely to everyone who needs them. The psychoactive/hallucinogenic effects, albeit shorter for some psychedelics, still requires trips to the clinic and supervision by a clinician. These limitations do restrict the ease of prescription for these life-changing compounds. Is this it for psychedelics? A flash in the pan? So full of potential, but so inaccessible.
Psychedelics 3.0
Enter psychoplastogens – the new and improved 3rd generation psychedelics without hallucinogenic and abnormal cardiac events. This is a truly remarkable pivot to design synthetic molecules that are the most effective and scalable, with the lowest adverse effects, and all at the comfort of the patient. Delix Therapeutics with their non-hallucinogenic, and Gilgamesh, Beckley Psytech, Diamond Tx, MagicMed Industries and CaamTech with their reduced-hallucinogenic compounds, will increase their market size by making them accessible to a larger proportion of the population.
In full disclosure, ARTIS Ventures recently led the $70M Series A for Delix Therapeutics, the leader in 3rd generation psychedelics. Delix has the potential to be the curative platform for mental health disorders, neurodegenerative disease and brain injury, and will move to clinical trials with its two leading compounds DLX-1, a MDMA analog, and DLX-7, an Ibogaine analog, next year. Both compounds are safe and effectively change the neuron architecture to be more connective, and greatly improve behavior in animal models of neuropsychiatric disorders. This may just be the inflection point in the treatment of depression and other disorders of the mind.
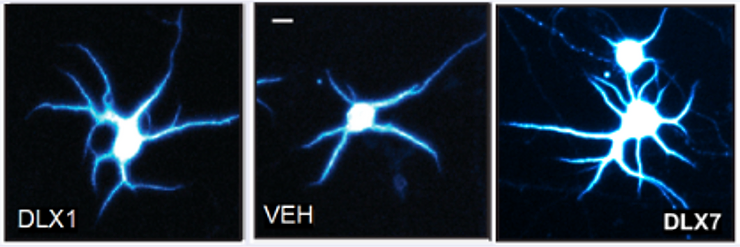
Image from Delix Therapeutics PreClinical Studies showing architecture of neurons treated with DLX-1, control (VEH) middle and DLX-7 showing neurogenesis; spinogenesis and dendritogenesis (growth of neuronal projections) associated with antidepressant effects.
"It felt like somebody had opened a window in a stuffy room.”
- Psilocybin clinical trial participant, Imperial College London
It is easy to fall into the hopeful traps of drug development, but psychedelics and psychoplastogens appear to increase the working and networking power of the neuron, and carry tremendous promise beyond depression and addiction disorders. While speculative and yet untested, the successful preventative use for neurodegenerative diseases that destroy the structure of the brain, like frontotemporal dementia, Parkinson’s and Alzheimer’s, or even migraines, will transform lives. Sub-hallucinogenic low doses of psychedelics, or microdosing, have grown in popularity due to perceived benefits of well-being and productivity. We must be cautious when we correlate neuronal growth after use of psychedelics and psychoplastogens to any functional benefits to the brain without rigorous studies. But if such a correlation can be made, will the enhanced neuronal circuitry augment our brain power? Stay tuned for this and more.
References:
- Marks, M., Cohen, I.G. Psychedelic therapy: a roadmap for wider acceptance and utilization. Nat Med 27, 1669–1671 (2021). https://doi.org/10.1038/s41591-021-01530-3
- https://www.healthypeople.gov/2020/topics-objectives/topic/mental-health-and-mental-disorders
- Zhdanava M, Pilon D, Ghelerter I, et al. The prevalence and national burden of treatment-resistant depression and major depressive disorder in the United States. J Clin Psychiatry. 2021;82(2):20m13699.
- Vahratian A, Blumberg SJ, Terlizzi EP, Schiller JS. Symptoms of Anxiety or Depressive Disorder and Use of Mental Health Care Among Adults During the COVID-19 Pandemic — United States, August 2020–February 2021. MMWR Morb Mortal Wkly Rep 2021;70:490–494. DOI: http://dx.doi.org/10.15585/mmwr.mm7013e2
- Tullis, Paul. "How ecstasy and psilocybin are shaking up psychiatry." Nature 589.7843 (2021): 506-509. https://media.nature.com/original/magazine-assets/d41586-021-00187-9/d41586-021-00187-9.pdf











